Summary:
 Diabetic retinopathy is damage that can occur at the back of the eye from diabetes. Diabetic retinopathy can include bleeding, leaking, formation of new blood vessels, or retinal detachment. Regular examinations and treatment when necessary can reduce the risk of vision loss dramatically. Good blood sugars and good blood pressures also reduce the risk of developing diabetic retinopathy by greater than 50%.
Diabetic retinopathy is damage that can occur at the back of the eye from diabetes. Diabetic retinopathy can include bleeding, leaking, formation of new blood vessels, or retinal detachment. Regular examinations and treatment when necessary can reduce the risk of vision loss dramatically. Good blood sugars and good blood pressures also reduce the risk of developing diabetic retinopathy by greater than 50%.
A more in-depth explanation of Diabetic Retinopathy
Diabetic Retinopathy Information PDF
What is diabetic retinopathy?
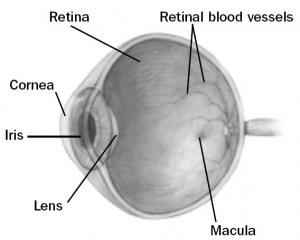 Diabetic retinopathy is a complication of diabetes and a leading cause of blindness. It occurs when diabetes damages the tiny blood vessels inside the retina, the light-sensitive tissue at the back of the eye. A healthy retina is necessary for good vision. If you have diabetic retinopathy, at first you may notice no changes to your vision. But over time, diabetic retinopathy can get worse and cause vision loss. Diabetic retinopathy usually affects both eyes.
Diabetic retinopathy is a complication of diabetes and a leading cause of blindness. It occurs when diabetes damages the tiny blood vessels inside the retina, the light-sensitive tissue at the back of the eye. A healthy retina is necessary for good vision. If you have diabetic retinopathy, at first you may notice no changes to your vision. But over time, diabetic retinopathy can get worse and cause vision loss. Diabetic retinopathy usually affects both eyes.
What are the stages of diabetic retinopathy?
Mild Nonproliferative Retinopathy
At this earliest stage, microaneurysms occur. They are small areas of balloon-like swelling in the retina’s tiny blood vessels. Moderate
Nonproliferative Retinopathy
As the disease progresses, some blood vessels that nourish the retina are blocked.
Severe Nonproliferative Retinopathy
Many more blood vessels are blocked, depriving several areas of the retina with their blood supply. These areas of the retina can produce chemical signals which can stimulate the growth of new abnormal retinal blood vessels.
Proliferative Retinopathy
At this advanced stage, the growth or proliferation of new abnormal blood vessels has occurred. This condition is called proliferative retinopathy. These new blood vessels are abnormal and fragile. They grow along the retina and along the surface of the clear, vitreous gel that fills the inside of the eye. By themselves, these blood vessels do not cause symptoms or vision loss. However, they have thin, fragile walls. If they leak blood, severe vision loss and even blindness can result.
Who is at risk for diabetic retinopathy?
All people with diabetes–both type 1 and type 2–are at risk. That’s why everyone with diabetes should get a comprehensive dilated eye exam at least once a year early in diabetes and more frequently as directed by their ophthalmologist. Approximately 25% of Canadians diagnosed with diabetes have some stage of diabetic retinopathy. If you have diabetic retinopathy, we may recommend treatment to help prevent worsening of your eye disease.
How does diabetic retinopathy cause vision loss?
Fluid can leak into the center of the macula, the part of the eye where detailed central vision occurs. The fluid makes the macula swell, blurring vision. This condition is called macular edema. It can occur at any stage of diabetic retinopathy, although it is more likely to occur as the disease progresses. About half of the people with proliferative retinopathy also have macular edema.
Fragile, abnormal blood vessels can develop and leak blood into the vitreous chamber in the center of the eye, blurring vision. This is called a vitreous hemorrhage. The abnormal blood vessels (neovascularization) that grow with proliferative retinopathy can contract and pull on the retina. In some cases this contraction can cause retinal detachment.
Does diabetic retinopathy have any symptoms?
Diabetic retinopathy often has no early warning signs. Don’t wait for symptoms. Make sure to keep your appointments and see your retina specialist as directed. However, possible symptoms can range from mild blurring of vision to sudden near complete visual loss.
How diabetic retinopathy treated?
In recent years there have been new advances in the treatment of diabetic retinopathy:
1) Focal retinal laser: Significant macular edema can often be treated with laser. The small leaky blood vessels are targeted and treated so they no longer leak. The procedure is not painful, although the laser light can be bright. It takes only a few minutes to do the procedure although it takes a few months for the eye to stop leaking. Often more than one treatment is needed to stop the leakage. New areas of leakage can develop or treated areas may start leaking again so continued follow up with your retina specialist is necessary. Focal laser treatment helps to preserve vision. In fact, focal laser treatment has been shown to reduce the risk of vision loss by 50 percent. It can also improve the vision in some people.
2) Pan retinal laser photocoagulation (PRP): This is an important treatment for proliferative diabetic retinopathy. The oxygen and nutrient starved peripheral retina produces the chemical signals that causes the abnormal blood vessels to grow. Ablation of the peripheral retina is performed with laser to shut down the production of this chemical signal. This allows the abnormal blood vessels to shrink away. More laser spots with more power are required for this treatment compared to focal laser. As a result, this procedure can sometimes be painful. Because a high number of laser spots are necessary, three or more sessions usually are required to complete treatment. Side effects of PRP can include loss of your side vision, color vision or night vision. However, it is an essential treatment to protect vision.
3) Injections: More recent research and experience has lead to the use of eye injections for the treatment of diabetic retinopathy. Both Lucentis® and Avastin® are used in the treatment of diabetic retinopathy. These medicines are injected into the eye. They act as chemical sponges to “sop up” and bind to the “bad” chemical signals that are released by the retina as result of diabetic damage. These medicines can be used to treat macular edema (swelling) and neovascularization (abnormal blood vessel growth).
4) Vitrectomy: The abnormal retinal blood vessels that develop as a result of diabetic retinopathy can bleed into the vitreous cavity of the eye. This can result in new floaters or significant sudden visual loss. In addition, to causing visual loss the blood can interfere with laser treatment of the retina. As a result, a surgery called a vitrectomy is required. A vitrectomy allows for removal of the blood from the eye and permits the surgeon to perform laser directly inside of your eye. Vitrectomy is also necessary to treat any significant traction on the retina produced by abnormal blood vessels. Your retinal surgeon will discuss this surgical procedure with you further if it is required.
What happens during laser treatment?
Both focal and pan retinal laser treatment are performed at our office or at the Royal Alexandra eye clinic. Before the laser, we will dilate your pupil and apply drops to freeze the front of the eye. The area behind your eye also may be frozen to prevent discomfort. The lights in the office will be dim. As you sit facing the laser machine, we will hold a special lens to your eye to prevent the lid from closing. During the procedure, you may see flashes of light. These flashes eventually may create a stinging sensation that can be uncomfortable. You will need someone to drive you home after laser. Because your pupil will remain dilated for a few hours, you should bring a pair of sunglasses. For the rest of the day, your vision will probably be a little blurry. If your eye has increasing pain or you develop nausea or vomiting, you should call our office.
What happens during the eye injections?
Anesthetic drops will be applied to freeze the surface of your eye. A speculum (spring) will be used to hold your eye open. An iodine solution will then be placed on the surface of the eye to sterilize it. You will be asked to look up or behind you to correctly rotate your eye. The medicine will then be injected by your specialist. It is normal to feel a sharp pinch, pressure or popping sensation at the time of the injection. Any discomfort is usually temporary. The remaining iodine solution will then be flushed from your eye. It is normal for the eye to be red after the procedure. New temporary floaters are also common.