An epiretinal membrane or wrinkle is a thin sheet of cells and/or vitreous jelly that is stuck on the retina. If vision is affected then surgery can be performed to remove the wrinkle and improve the vision in most cases. The risk of surgery includes cataract formation and retinal detachment. If surgery is performed it can take 6 months to 1 year for vision to improve.
A more in-depth explanation of Epiretinal Membrane
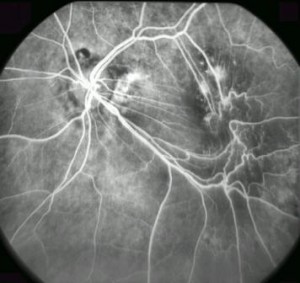
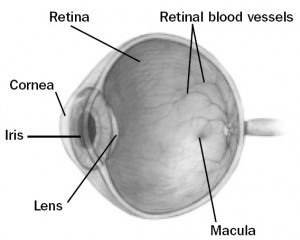 An epiretinal membrane (also known as a macular pucker or cellophane maculopathy) is a condensation of a fibrous “membrane” on the surface of the retina. Often it is a result of the vitreous (Jelly that fills the eye) contracting and pulling off from the back surface of the eye. When it does so, it can leave a sheet of vitreous behind, like the skin of an onion stuck on the retina. Different types of cells can then multiply and cause further contraction of this sheet of vitreous on the surface of the retina. The “macula” is the center of the retina where the highest visual acuity is obtained. This is the part of the retina that is crucial for reading and detailed central vision. Membranes can cause the surface of the macula to become wrinkled and more opaque, like a layer of plastic wrap over a camera film. This can cause distortion or blurring of central vision.
An epiretinal membrane (also known as a macular pucker or cellophane maculopathy) is a condensation of a fibrous “membrane” on the surface of the retina. Often it is a result of the vitreous (Jelly that fills the eye) contracting and pulling off from the back surface of the eye. When it does so, it can leave a sheet of vitreous behind, like the skin of an onion stuck on the retina. Different types of cells can then multiply and cause further contraction of this sheet of vitreous on the surface of the retina. The “macula” is the center of the retina where the highest visual acuity is obtained. This is the part of the retina that is crucial for reading and detailed central vision. Membranes can cause the surface of the macula to become wrinkled and more opaque, like a layer of plastic wrap over a camera film. This can cause distortion or blurring of central vision.
ERMs can be associated with a variety of eye conditions, retinal tears, retinal detachments, eye inflammation, and vitreous hemorrhage. However, large proportions ERMs occur without any previous eye problems.
Visual acuity decreases to a level depending on how distorted the macular surface becomes. Some patients will have minimal vision distortion; others may have severe loss to the level of legal blindness. Sometimes even though your vision reading the eye chart may be quite good, the vision will still functionally be very poor due to distortion (straight lines appear bent, wrinkled).
The decision on trying to repair the membrane depends on how impaired vision has become. This is often determined by whether or not you can read with that eye alone (ie. Cover your good eye). If untreated the epiretinal membrane may remain stable or may continue to increase its distortion and cause further vision loss in the eye.
What can be done for an epiretinal membrane?
When vision is significantly impaired a surgical procedure called an vitrectomy and membrane peel can be performed. This procedure involves the removal of the vitreous gel from the eye. The epiretinal membrane is then gently grasped and peeled from the surface of the macula. Once the membrane is removed the traction on the retina is relieved and the macula can begin to flatten and become smoother. The vitreous gel is replaced with a special saline fluid during surgery and gradually your body replaces it with naturally produced fluid. Sometimes your retinal surgeon will decide to replace the vitreous with an air or gas bubble to help flatten the retina. The air bubble gradually goes away on its own and is replaced by the eyes normal intraocular fluid. Three small self-sealing incisions are made into the eye to perform the surgery. Occasionally, dissolving sutures are used.
What can I expect after surgery?
There is usually very little pain. It is common for patients to experience mild irritation for a few days after surgery. The use of an eye patch is recommended for 3 days. You will be given an eye shield which should be worn while sleeping for approximately 1 week. You will be given a prescription for eye drops to be used for 2–4 weeks. Severe pain or nausea and vomiting are indications to call your surgeon immediately. The eyelids are usually swollen for the first couple of weeks, but this gradually resolves thereafter. Vision is often very blurry for the first few days. An improvement in vision usually takes a few months to be noticed. Vision will usually slowly continue to improve in the months following surgery and can take up to 2 years to be maximally improved.
What are the risks of the procedure?
There are always risks associated with surgical procedures. A retinal detachment occurs in about 1-3% of patients but is usually treatable with further surgery. The intraocular pressure is transiently elevated in about 20% of patients. This is usually well controlled with eye drops and temporary. However, the inconvenience of additional office visits or medical therapies may be necessary.
The most severe complications occur less frequently: the risk of severe hemorrhage, infection, irreparable retinal detachment or complications from anesthesia occurs in approximately one in several thousand cases. These complications could result in irreversible blindness. Rarely double vision or eyelid droop may develop and need to be repaired with further surgery.
The most common side effect of epiretinal membrane surgery is cataract development. Cataract is a side effect of vitrectomy surgery, regardless of the underlying diagnosis. It often begins to develop by 6 to 12 months after surgery; however, it can develop sooner. If necessary, it can be surgically removed in the future, and an intraocular lens can be implanted.
The risks of the procedure are far outweighed by the benefits to your vision by removing the membrane. Usually we expect a significant improvement in both visual acuity and central distortion.
What follow-up is necessary?
For the benefit of the patient, it is important to monitor the status of the eye following surgery. We usually see the patient one day, 1-2 weeks, 6-8 weeks, and then 3 or 4 months after surgery. These may be modified by your doctor. We will give you written directions after surgery about the care of your eye and follow up appointments. After surgery you should expect your eye to be red. If there is increasing pain or a perceived significant decrease in vision or other concerns you should call our office at (780) 448-1801. If it is after weekday hours or on the weekend the answering service will page the retina specialist on call for our office.