Summary:
 Macular holes develop because of traction on the central retina by the vitreous. Surgical treatment to remove the vitreous from the eye followed by injection of a gas bubble is successful in repairing the hole 90-95% the time. Without surgery, a macular hole will not improve.
Macular holes develop because of traction on the central retina by the vitreous. Surgical treatment to remove the vitreous from the eye followed by injection of a gas bubble is successful in repairing the hole 90-95% the time. Without surgery, a macular hole will not improve.
A more in-depth explanation of macular holes
What is a “Macular Hole”?
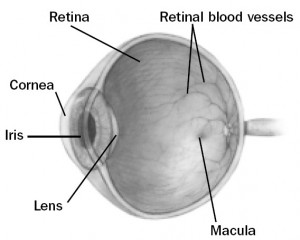 The “macula” is the center of the retina where the highest visual acuity is obtained. A macular hole is a full thickness defect in this important location of the retina. This is like a hole in the center of the film in your camera. This hole is the result of traction of the vitreous on the retina. The vitreous is a jelly-like substance which fills the central cavity of the eye. In some the vitreous is firmly attached to the macula. As the vitreous “shrinks” and “collapses” with age it can pull on the center of the macula. This oblique traction can open a full thickness defect in the center of the macula (fovea). There is no actual loss of tissue in the hole. Visual acuity decreases markedly to a level depending on the size of the hole, but usually to the level of legal blindness. Visual loss is due to disruption of the normal physiologic arrangement of the photoreceptors (light sensing cells) in the center of the macula, and due to collection of fluid under the retina in this area.
The “macula” is the center of the retina where the highest visual acuity is obtained. A macular hole is a full thickness defect in this important location of the retina. This is like a hole in the center of the film in your camera. This hole is the result of traction of the vitreous on the retina. The vitreous is a jelly-like substance which fills the central cavity of the eye. In some the vitreous is firmly attached to the macula. As the vitreous “shrinks” and “collapses” with age it can pull on the center of the macula. This oblique traction can open a full thickness defect in the center of the macula (fovea). There is no actual loss of tissue in the hole. Visual acuity decreases markedly to a level depending on the size of the hole, but usually to the level of legal blindness. Visual loss is due to disruption of the normal physiologic arrangement of the photoreceptors (light sensing cells) in the center of the macula, and due to collection of fluid under the retina in this area.
What can be done for a macular hole?
Up until about 1992, there was nothing that could be done to alter the status of a macular hole. We now perform a surgical procedure that involves removing the vitreous gel and internal limiting membrane (the innermost layer of the retina) from the eye to relieve any traction and distortion of the macula. When the traction is relieved the macula can “relax” back into its normal anatomical position which closes the macular hole.
The vitreous gel is replaced with a mixture of air and a slowly dissolving inert gas (C3F8 or SF6) at the end of your surgery. The surface tension of the gas bubble acts to aid in closure of the macular hole. In order to maximize the effect of the bubble, you may be requested to maintain face down (prone) positioning or positioning on your side positioning for a period of time after your surgery. This ensures that the gas bubble will stay in contact against the macular hole. Your surgeon will discuss your positioning instructions with you.
What can I expect after surgery?
Gas placed within the eye will be gradually reabsorbed by the eye during a 2-8 week period following surgery. As the bubble is reabsorbed, the vitreous cavity refills with a fluid that is naturally produced by the eye. Vision will be markedly reduced immediately after surgery since you cannot see well through the bubble. As the bubble reabsorbs you will gradually see more and more. You should not, however, expect to experience significant improvement in vision until at least 6 weeks after surgery, and final visual acuity outcome may not be obtained for up to 2 years following the macular hole repair. You may not fly in an airplane or travel to high elevations (i.e. mountains) until the bubble is almost completely gone. Some types general anesthetic agents must be avoided (nitrous oxide or laughing gas) while there is a gas bubble in your eye.
There is usually very little pain. It is common for patients to experience mild irritation for a few days after surgery. The use of an eye patch is recommended for 3 days. You will be given an eye shield which should be worn while sleeping for approximately 1 week. You will be given a prescription for eye drops to be used for 2–4 weeks. Severe pain or nausea and vomiting are indications to call your surgeon immediately, even if it is the evening or weekend. It may be an indication that the pressure in the eye is too high. The eyelids are usually swollen for the first couple of weeks, but this gradually resolves thereafter. As the gas bubble shrinks in your eye, you will begin to notice a fluid level when looking through the operated eye. This level will gradually change with time. Often, satellite bubbles will form, giving the appearance of fish eggs or small balloons when you look through the operated eye. This is normal and is no cause for alarm.
What are the risks of the procedure?
There are always risks associated with surgical procedures. A retinal detachment occurs in about 1-3% of patients but is usually treatable with further surgery, often with little or no adverse effect on your final vision. The intraocular pressure is transiently elevated in about 20% of patients. Often a feeling of nausea or eye pain will accompany elevated intraocular pressure. This is usually well controlled with eye drops and temporary. However, the inconvenience of additional office visits or medical therapies may be necessary.
The most severe complications occur less frequently: the risk of severe hemorrhage, infection, irreparable retinal detachment or complications from anesthesia occurs in approximately one in several thousand cases. These complications could result in irreversible blindness. Rarely double vision or eyelid droop may develop and need to be repaired with further surgery.
The most common side effect of macular hole surgery is cataract development. A cataract is a side effect of vitrectomy surgery, regardless of the underlying diagnosis. It begins to develop in almost all patients by 6 to 12 months after surgery; however, it may develop sooner. If necessary, it can be surgically removed in the future, and an intraocular lens can be implanted.
The risks of the procedure are far outweighed by the benefits to your vision by repairing the macular hole. Up to 15% of patients may develop a macular hole in their other eye, or suffer vision loss in their other eye from some other cause Therefore, repair of the macular hole is very important.
What follow-up is necessary?
For the benefit of the patient, it is important to monitor the status of the eye following surgery. We usually see the patient one day, 1-2 weeks, 6-8 weeks, and then 3 or 4 months after surgery. These may be modified by your doctor. We will give you written directions after surgery about the care of your eye and follow up appointments. After surgery you should expect your eye to be red. If there is increasing pain or a perceived significant decrease in vision or other concerns you should call our office at (780) 448-1801. If it is after weekday hours or the weekend the answering service will page the retina specialist on call for our office.