Summary:
 Retinal detachments develop as a result of traction on the retina by the vitreous that first creates a retinal hole, then with continued traction leads to a retinal detachment. Treatment includes removing the vitreous from the eye with a gas bubble and laser or placing a silicone band around the eye, with a gas bubble and a freezing probe. Given enough time, all vision will be lost without surgery. Surgery is successful in approximately 85% of cases, with repeat surgery leading to re-attachment of the retina in 95% of cases.
Retinal detachments develop as a result of traction on the retina by the vitreous that first creates a retinal hole, then with continued traction leads to a retinal detachment. Treatment includes removing the vitreous from the eye with a gas bubble and laser or placing a silicone band around the eye, with a gas bubble and a freezing probe. Given enough time, all vision will be lost without surgery. Surgery is successful in approximately 85% of cases, with repeat surgery leading to re-attachment of the retina in 95% of cases.
A more in-depth explanation of Retinal Detachments
What is a retinal detachment?
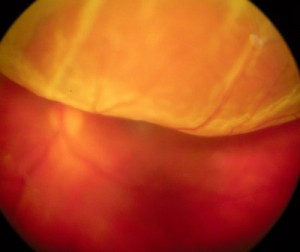
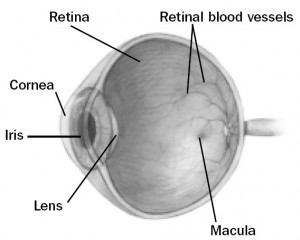 The inside of the eye is filled with a gel like substance called the vitreous. The vitreous has a jello or egg-white consistency when we are young, and is firmly attached to the front of the eye on the inside (called the vitreous base). The retina is the very thin tissue that lines the inside of the eye cavity like wallpaper. When we look at something, the retina acts like the film in a camera and captures the image. The retina is attached to the wall of the eye only at the very front and at the back of the eye where the optic nerve goes to the brain. The vitreous is more lightly attached to the rest of the retina. Over time, the vitreous gradually becomes thinner and more liquified. It eventually collapses inwards, and separates from the retina. This separation of the vitreous from the retina is called a posterior vitreous detachment (PVD). PVD’s are typically harmless and cause increased floaters in the eye. In some cases, the traction on the retina may create a tear. Retinal tears frequently lead to retinal detachment as fluid from the vitreous seeps underneath the retina. This fluid causes the retina to separate and detach from the outer layers of the eye. Retinal detachment can also develop from holes in the peripheral retina which develop in areas of retinal thinning.
The inside of the eye is filled with a gel like substance called the vitreous. The vitreous has a jello or egg-white consistency when we are young, and is firmly attached to the front of the eye on the inside (called the vitreous base). The retina is the very thin tissue that lines the inside of the eye cavity like wallpaper. When we look at something, the retina acts like the film in a camera and captures the image. The retina is attached to the wall of the eye only at the very front and at the back of the eye where the optic nerve goes to the brain. The vitreous is more lightly attached to the rest of the retina. Over time, the vitreous gradually becomes thinner and more liquified. It eventually collapses inwards, and separates from the retina. This separation of the vitreous from the retina is called a posterior vitreous detachment (PVD). PVD’s are typically harmless and cause increased floaters in the eye. In some cases, the traction on the retina may create a tear. Retinal tears frequently lead to retinal detachment as fluid from the vitreous seeps underneath the retina. This fluid causes the retina to separate and detach from the outer layers of the eye. Retinal detachment can also develop from holes in the peripheral retina which develop in areas of retinal thinning.
Retinal detachment is a serious problem and can result in permanent visual loss. It is a medical emergency and anyone experiencing symptoms of retinal detachment should seek assessment from an eye care professional immediately.
What are symptoms of retinal detachment?
The initial symptoms of retinal detachment may be quite mild. A sudden onset of flashing lights and multiple new floaters (little “cobwebs” or specks that float about in your field of vision) may occur. Flashes and floaters are often the symptoms of a retinal tear. After a retinal tear has occurred the retina may begin to detach. As the retina starts to detach changes in peripheral vision (outside vision) in one eye begin to occur. Loss of peripheral vision from the side top or bottom may advance towards the center of vision like a curtain, often in a “half moon” shape. This can progress to total vision loss. Sometimes, the symptoms of retinal detachment may go unnoticed until central vision is affected. Occasionally, a peripheral retinal detachment may be present without producing any symptoms at all. This is one reason regular eye exams with your ophthalmologist are very important.
Who is at risk for retinal detachment?
A retinal detachment can occur at any age, but it is more common in people over age 40. You should discuss your risk for retinal detachment with your ophthalmologist. Risk factors for retinal detachment include:
- Myopia (nearsightedness)
- Previous retinal detachment in the other eye
- Family history of retinal detachment
- Cataract surgery
- Eye trauma
- Other predisposing eye diseases or disorders
- Predisposing genetic conditions
How are retinal detachments repaired?
Retinal detachment can only be repaired with a surgical procedure. Your retinal specialist will discuss your surgery with you. There are three main types of surgical procedures for retinal detachment repair.
- Pneumatic retinopexy: This procedure is used to treat retinal detachments with very specific characteristics. A temporary gas bubble is injected into the vitreous cavity of the affected eye. The surface tension of the gas bubble acts to seal off the retinal tear or hole. Your eye can then pump out the fluid that has accumulated under the retina. The success of this procedure requires strict positioning of your head after the gas injection to ensure that the bubble seals off the retinal break. The retinal tear is directly treated with cryopexy (a super cooled probe applied to the outside of the eye) or retinal laser to prevent the detachment from returning once the bubble is absorbed by your eye.
- Scleral buckle: This is the type of procedure most commonly used for people who have a retinal detachment but have not had cataract surgery yet. All retinal tears are directly treated with cryopexy (a super cooled probe applied to the outside of the eye). A silicone band is then placed around the outside of the eye behind the insertion of the 4 major muscles that move the eye. This indents the eye wall to move it closer to the retina. This acts to release the pulling of the vitreous gel on the retina to allow closure of retinal breaks. Fluid is then removed from the front of the eye to decrease pressure inside the eye. Finally, a temporary gas bubble is injected into the eye. The surface tension of the gas bubble acts to seal off the retinal tear or hole. Following the surgery your retinal specialist may ask you to position your head in a specific way.
- Pars plana vitrectomy: This is the type of procedure most commonly used for people who have a retinal detachment and have had prior cataract surgery. Three small incisions are made through the sclera (the white of the eye). Your surgeon then uses a microscope and a special lens system to operate directly within your eye. A special instrument, called a vitrector, is used to remove as much vitreous gel as possible. This eliminates any traction on the retina. The fluid under the detached retina and within the vitreous cavity is then drained. A probe is then inserted into the eye so that laser can be used to permanently seal off any retinal breaks. A slow absorbing gas is then injected into the eye to completely fill up the vitreous cavity. The surface tension of the gas acts to seal of the retinal breaks while the laser spots are maturing. Your surgeon may request that you position your head in a specific way after the surgery to position the gas bubble onto the retinal breaks and detached retina. The gas bubble will be slowly absorbed by your eye at different rates depending on the type of gas used. Sometimes silicone oil is placed within the vitreous cavity instead of gas. If this is the case, a second surgery is usually required to remove the oil. Sometimes, a combination of both scleral buckle and vitrectomy surgeries will be performed. Your retinal specialist will discuss which surgery will be best for you.
What is intraocular gas and silicone oil?
Gas placed within the eye will be gradually reabsorbed by the eye during a 2-8 week period following surgery. As the bubble is reabsorbed, the vitreous cavity refills with a fluid that is naturally produced by the eye. Vision will be markedly reduced immediately after surgery since you cannot see well through the bubble. As the bubble reabsorbs you will gradually see more and more. You should not, however, expect to experience significant improvement in vision until at least 6 weeks after surgery, and final visual acuity outcome may not be obtained for up to 2 years following the retinal detachment repair. You may not fly in an airplane or travel to high elevations (i.e. mountains) until the bubble is almost completely gone. Some types general anesthetic agents must be avoided (nitrous oxide or laughing gas) while there is a gas bubble in your eye.
Silicone oil does not reabsorb on its own, instead it must be removed with an additional surgical procedure from 2 months to 2 or more years after the original surgery. If silicone oil is utilized, there is no risk from flying or from having a general anesthetic.
Over 90% of retinal detachments can be successfully treated. However often more than one procedure is necessary. Unfortunately, even after multiple attempts at retinal detachment repair, treatment sometimes fails and vision may be lost permanently. Visual outcome is not always predictable. Visual results are usually best if the retinal detachment is repaired before the macula (the center region of the retina responsible for fine, detailed vision) detaches. This is why urgent surgery is often required. The final visual result may not be known for up to several months following surgery.
What can I expect after surgery?
The eye may be quite sore for approximately 1 to 2 weeks following sclera buckling surgery. There is usually very little pain following pneumatic retinopexy and vitrectomy procedures. However, it is common for patients to experience mild irritation for a few days after surgery. The use of an eye patch is recommended for 3 days, or until the eye stops tearing. You will be given an eye shield which should be worn while sleeping for approximately 1 week. You will be given a prescription for eye drops to be used for 2–4 weeks. Severe pain or nausea and vomiting are indications to call your surgeon immediately even if it is the evening or weekend. The eyelids are usually swollen for the first couple of weeks, but this gradually resolves thereafter. As the gas bubble shrinks in your eye, you will begin to notice a fluid level when looking through the operated eye. Some vision should be present above the fluid level. The top field of vision should gradually enlarge as the bubble shrinks. Often, satellite bubbles will form, giving the appearance of fish eggs or small balloons when you look through the operated eye. This is normal and is no cause for alarm. If your vision is good one day, then much worse the next, you may have developed a recurrent retinal detachment. You should contact our office immediately, even if it is the evening or weekend.
What follow-up is necessary?
For the benefit of the patient, it is important to monitor the status of the eye following surgery. We usually see the patient one day, 1-2 weeks, 6-8 weeks, and then 3 or 4 months after surgery. These may be modified by your doctor. We will give you written directions after surgery about the care of your eye and follow up appointments. After surgery you should expect your eye to be red. If there is increasing pain or a perceived significant decrease in vision or other concerns you should call our office at (780) 448-1801. If it is after weekday hours or the weekend the answering service will page the retina specialist on call for our office.