Summary:
A branch retinal vein occlusion (BRVO) is a blockage of one of the blood vessels in the retina. Risk factors include arteriosclerosis, high blood pressure and diabetes, although many people who develop BRVOs do not have any of these risks. BRVOs can lead to leakage of the retina that can reduce vision, and to new blood vessels that can break and bleed. Treatment includes injections of medication into the eye and laser treatment.
A more in-depth explanation of Vein Occlusions
What Is A Branch Retinal Vein Occlusion?
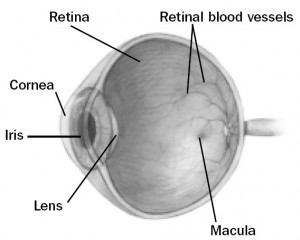 A branch retinal vein occlusion (BRVO) is a blockage of one of the small blood vessels that drains blood from the retina. The retina is the light-sensitive nerve tissue lining the back of the eye.
A branch retinal vein occlusion (BRVO) is a blockage of one of the small blood vessels that drains blood from the retina. The retina is the light-sensitive nerve tissue lining the back of the eye.
Like film in a camera, the retina continually “takes pictures” of everything you look at. When part of the retinal vein becomes blocked, the retinal blood flow slows or stops. Suddenly and usually without warning, a patch of retina loses some of its “picture-taking” function and you may be aware that part of your field of vision has darkened.
Why Is Vision Lost?
Normally, the retina is nourished by oxygen-rich blood that is brought to it by arteries and drained away by veins. When a vein – a drainage channel – is blocked, blood backs up, leading to bleeding and swelling (edema) in the retina which hampers its nourishment.
The extent of damage and the visual symptoms produced depend on the size of the blocked vein and its exact location. If the blockage occurs toward the peripheral part of the retina, you may hardly notice it. But if it occurs in or near the macula – the central zone of the retina that is critical for sharp vision – and causes it to swell, vision is likely to be reduced or distorted.
A more serious threat to vision can develop later from a complication called neovascularization (neo = new, vascular = blood vessels). A month or more after the BRVO, new blood vessels may begin to appear in the retina, as if they were trying to renourish it. These are not normal blood vessels as they are very fragile and bleed easily. They are dangerous to the eye because they can lead to still other problems that damage vision.
Neovascularization only occurs in about one in five BRVO patients. If it develops in your eye, it should be treated before causing harm. In most cases there are no warning symptoms; but occasionally there are, such as the sudden appearance of new floaters (translucent specks that move about in your field of vision) or a sudden decrease in vision.
What Causes a Vein Occlusion?
Several factors combine to bring on an occlusion. The usual situation is that something causes the blood flow in a retinal vein to slow down so much that it permits a clot to form there. The clot prevents blood from flowing freely.
The most common reason for slowed venous blood flow is, surprisingly, a hardened artery (arteriosclerosis). If a stiff artery happens to lie across a vein and compresses it, it can slow the flow of blood in that vein in the same way that stepping on a hose can obstruct the flow of water. Because arteriosclerosis occurs so often in people who have hypertension (high blood pressure), and diabetes they are considered to be a risk factor for the development of BRVO.
Other conditions that can lead to a BRVO are venous inflammation (vasculitis), which can plug the vein , and some rare blood conditions that produce a greater-than-normal tendency for blood to clot. Even estrogen medication (as in oral contraceptives) can introduce a slight risk of blood clotting.
In many cases no risk factors are found and simply the way your individual blood vessels lay one atop the other puts you at risk as you age.
Retinal photographs may be taken to help determine the extent of the problem. An angiogram (photographs of blood vessels) may also be done. For this test, an orange-colored dye (fluorescein) is injected into a vein in your arm and is immediately followed by a series of retinal photographs that track the dye, and time its flow, as it travels through the eye’s blood vessels. The angiogram helps identify the exact site of the vein’s blockage, the extent of damage to capillaries (the smallest retinal blood vessels), the site of leakage and whether or not neovascularization has developed. OCT (optical coherence tomography) scans will be performed to monitor the position and extent of swelling within the retina.
Because BRVO can be associated with medical conditions that affect the rest of the body (high blood pressure, for example, which also increases the risk of a heart attack or stroke), you should be evaluated by our ocular stroke clinic. Our office will arrange this for you. (if not let us know so we can do so).
Treatment
Once a BRVO has occurred; there is no simple way to speed the healing process along. Eventually, over several months, the blocked vein may re-open on its own, or some nearby blood vessels (called collaterals) may develop and reroute the blood flow around the site of blockage. Either of these may help restore at least part of the lost retinal function.
If neovascularization develops, a type of laser surgery called panretinal photocoagulation (PRP) can help reduce or even eliminate the abnormal blood vessels. PRP is not intended to improve vision directly. It reduces the risk of further vision loss from internal bleeding or, possibly, from a retinal detachment.
After a BRVO, the central retina (macula) sometimes remains swollen for months, reducing vision significantly. You may be treated with eye injections of special medicines called Avastin and Lucentis to help resolve or reduce the swelling, often more than once. These medicines were initially developed to treat wet age related macular degeneration. However, they are also very effective in reducing macular swelling (edema) caused by BRVO. Laser treatments may also be used to minimize the macular swelling. Your doctor will discuss these treatments with you.
Regular follow-up examinations are important to protect your eyesight. Your eyes should be checked regularly for potential late complications, such as neovascularization or macular edema, and for the development of a second vascular occlusion in either eye.